ICHRAs — Individual Coverage Health Reimbursement Arrangements — are an employer-provided group health benefit changing how employees get health insurance.
ICHRAs benefit everyone, offering a powerful alternative to traditional group health benefits because they provide:
- Greater cost control for employers
- Freedom of choice for employees
- A way for brokers to retain business amid unsustainable group rate increases
In this article, we break down ICHRA benefits for employees, employers, and brokers and share how ICHRA administration is simple with technology like Nexben’s patent-pending payment solution.
What is an ICHRA?
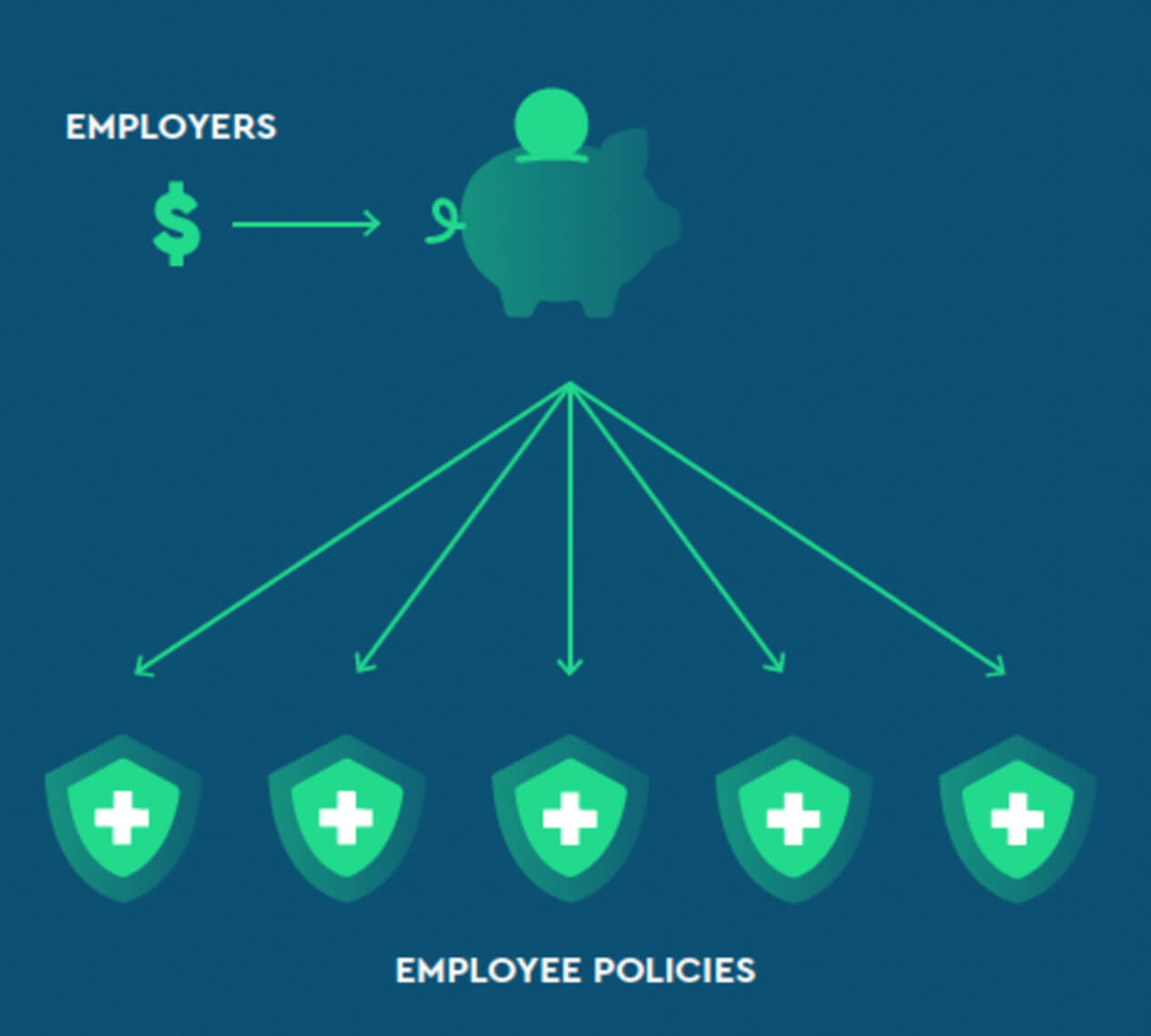
An ICHRA (sometimes called a defined contribution approach) is an employer-funded, tax-free health benefit used to reimburse employees for individual health insurance premiums and other qualified medical expenses. Employers set a monthly contribution amount for each employee, and employees use that contribution to shop for an individual policy that best fits their needs.
ICHRAs are different from traditional group health insurance (sometimes called a defined benefit approach), where employers select a one-size-fits-most group plan that typically limits employees to one to three policies.
ICHRA benefits for employees
ICHRAs offer three key benefits to employees:
1. Offers more choice in coverage options
In a traditional group plan, employees typically only get to choose from one to three health insurance policies. However, when offered an ICHRA, employees can select whichever policy from the individual health insurance marketplace best fits their needs. In 2025, over 9 insurers are participating in the individual marketplaces in each state— providing significantly more coverage choices to employees than a group plan.
2. Presents tax advantages
The monthly contributions that employers offer their employees are pre-tax funds. In other words, employees get help paying for their health insurance coverage without the funds increasing their taxable income.
In many cases, the same is true for any remaining balance that an employee is responsible for after their employer’s contribution: the remaining amount can be deducted from the employee’s paycheck, pre-tax.
3. Provides coverage portability
Because the policies purchased through an ICHRA are individual policies, employees can take the coverage with them if they leave the company.
The Nexben experience for employees
Shopping for, enrolling in, and paying for an individual health insurance policy is simple when employees get access to Nexben:
- Employees get access to their employer’s contribution through a unique bank account (not a debit card). This bank account is important because it ensures a secure and compliant payment transfer and because not all carriers accept payment via a credit or debit card.
- Employees do not have to front the full premium cost and then wait for their employer to reimburse them.
- If employees choose a policy that costs more than the employer’s contribution, the remainder may be payroll deducted pre-tax.
- Selecting an individual policy is a new experience for many employees. With Nexben, employees get access to benefits experts who can help them shop for, evaluate, and choose the plan that makes the most sense for them.
ICHRA benefits for employers
ICHRAs have historically made the most sense for small employers with 50 or fewer employees. However, they’re now just as relevant for large employers, with Applicable Large Employers (ALEs) being the fastest-growing ICHRA segment.
1. Enables controlled healthcare costs
These defined contributions are the maximum amount an employer will spend each month. Any contribution amounts not used by employees are forfeited and may be available to the employer to contribute to other policy types or to pay plan expenses.
With ICHRAs, employers are no longer at the whim of steep and unpredictable group rate increases and can confidently set their benefits budgets year after year.
2. Eliminates the burden of choosing coverage for employees
marketplace that an employer already uses or wants to use.
Eliminating this significant decision allows businesses more time to focus on what they do best instead of navigating the complex world of health benefit design and administration.
3. Works as a recruitment and retention tool
4. Reduces administrative stress
5. Can be started at any time during the year
The Nexben experience for employers
- Employers add employee data via a simple spreadsheet upload to their Nexben account.
- Employees can work directly with brokers and enrollment advocates (not the employer’s HR team) to select the individual coverage that fits their needs best.
- Employers click one button to pay a single invoice that combines all of their employees’ premiums. Nexben’s payment technology distributes all defined contributions across all employee benefit plans, regardless of how many different insurance carriers employees choose from.
- Nexben provides necessary reports to support payroll and ACA reporting requirements.
- Employers pay Nexben an administrative fee per enrollee per month for the employees actively using the platform. Any size group can leverage Nexben’s payment solution without minimum enrollment requirements or setup and renewal fees.
ICHRA benefits for brokers & distribution partners
Some brokers and distribution partners still get a little spooked by ICHRAs. But the most forward-thinking among them are learning why it’s so critical to embrace ICHRAs— and just how much ICHRAs can offer their business. Here are the key ICHRA benefits for brokers and distribution partners:
1. Retain clients that can’t sustain group rate increases
If brokers don’t present ICHRAs as an option to their clients, they will likely find the option elsewhere. By partnering with a payment technology company like Nexben, brokers can retain their status as agent of record on employee plans while offering their clients a compelling solution that helps them control costs.
2. Get the flexibility to choose enrollment involvement
The Nexben experience for brokers & distribution partners
- The broker’s role is to help clients develop an effective ICHRA strategy that lowers or stabilizes the company’s healthcare costs, satisfies affordability requirements (if applicable), and still provides employees with a strong benefit package.
- Brokers and distribution partners get access to the Nexben platform, where they can invite new employer groups to Nexben and track their clients’ enrollment statuses.
- Brokers and distribution partners also get access to Nexben’s partner portal, which includes learning modules and resources about ICHRAs and information about how Nexben works. More personalized, hands-on guidance is available via our partner success team.
About Nexben
Nexben is a financial technology company that helps employers, brokers, and distribution partners reap all ICHRA benefits. Get in touch if you’d like to learn more about how offering Nexben can help you deliver the best options to your employer clients and their employees.

